Among the many known diseases are most of them Musculoskeletal disorders are common, which is mainly associated with a lack of exercise. In addition, such problems are inherent not only in the elderly, but also in young people. Osteochondrosis of the cervical spine occupies a special place among diseases of the musculoskeletal system. What is this diseaseWhat does it threaten its owner with? How is it expressed? Are there any effective prevention and treatment measures?
Musculoskeletal disorders are common, which is mainly associated with a lack of exercise. In addition, such problems are inherent not only in the elderly, but also in young people. Osteochondrosis of the cervical spine occupies a special place among diseases of the musculoskeletal system. What is this diseaseWhat does it threaten its owner with? How is it expressed? Are there any effective prevention and treatment measures?
Cervical osteochondrosis is a degenerative-dystrophic progressive disease that is accompanied by deformation of the intervertebral discs. It requires immediate treatment to prevent irreversible pathological changes. Among the various forms of osteochondrosis, cervical pathology ranks second, only second after damage in the lumbosacral area.
Disease stages
The development of cervical osteochondrosis occurs in stages:
- First stage. Intervertebral discs begin to collapse: cracks appear in the annulus fibrosus, the intervertebral disc loses its strength and elasticity and becomes smaller. This compresses the nerve roots, which is accompanied by aching pain.
- Second floor. The destruction of the intervertebral disc continues, causing minor dislocations of the vertebrae. Sensations of pain intensify and become permanent. Falling head syndrome can develop, which is characterized by severe pain that forces the head to be held in a fixed position.
- Third section. The annulus fibrosus is almost completely destroyed, resulting in protrusions and herniated discs. In this case, the pain may decrease because there is no source of pain - cartilage tissue. But the pain syndrome does not go away completely because the nerve roots remain pinched. Possible violation of sensitivity, appearance of headache and dizziness, nausea, "lumbago" in the neck.
In the first stage, the disease is successfully cured. In the second and third stages, irreversible changes take place. Therefore, it is not possible to fully restore the body.
Causes of pathological changes
The vertebrae in the cervical spine are the most flexible. They are small and have weak muscles. This structure of the vertebrae contributes to the development of degenerative diseases. In addition, the neck region is saturated with nerves and blood vessels, the damage of which not only causes unpleasant symptoms, but also causes serious complications.
The main factors that lead to the development of cervical osteochondrosis include:
- sedentary lifestyle;
- prolonged stay in the same position;
- Metabolic disorders;
- Salt deposits;
- poor diet.
The risk of illness increases with:
- hereditary predisposition;
- high age;
- Neck injury;
- prolonged or regular hypothermia of the body;
- hormonal imbalance;
- Obesity;
- Autoimmune diseases;
- chronic musculoskeletal disorders.
Symptoms of the disease
The development of cervical osteochondrosis is slow. Symptoms of the disease depend on how many vertebrae are affected, the degree of damage, and the presence of pinched nerves.
The main symptom of the pathology is pain of varying intensity in the neck, radiating to the back of the head, ears, shoulders, forearms and chest. They are reinforced by turning the head and with the least amount of physical exertion.
In addition to pain in cervical osteochondrosis:
- Headache and heartache occur;
- dizzy;
- darkens in the eyes;
- Hands and feet are numb;
- Tinnitus can be heard;
- the tongue becomes numb;
- Visual acuity and hearing are weakened;
- a sharp turn of the head leads to unconsciousness;
- there is quick fatigue;
- coordination is disturbed.
Several syndromes of cervical osteochondrosis are known:
- radicular - pinching the nerve endings leads to severe pain in the neck, radiating to the shoulders, forearms, shoulder blades and lower back;
- Heart - the root of the chest muscle or phrenic nerve is damaged, causing symptoms similar to a heart attack: persistent pain in the chest area (it does not go away with taking nitroglycerin) that increases with exercise and deep breathing;
- vertebral artery - throbbing pain develops in the back of the head and temples;
- Irritant reflex - Burning pain occurs in the neck area, which radiates to the shoulder and chest area and is aggravated by coughing and turning the head.
Possible complications
Cervical osteochondrosis can cause significant damage to the body. It's especially dangerous because deformed vertebrae damage the nerve roots and blood vessels that carry blood to the brain. As a result, the brain does not receive the required amount of oxygen and nutrients, which can lead to disability and even death due to impaired cardiac activity and respiratory function.
Without the necessary treatment, the disease can lead to a wide variety of complications: vertebral artery syndrome, bulging, herniated disc, stroke, cerebral ischemia. Often, cervical osteochondrosis causes radiculopathy. In this case, growths form on the damaged vertebrae, as a result of which the body loses some or all of its sensitivity and mobility.
But the most dangerous compression of the spinal cord that leads to death.
Therefore, timely treatment for cervical osteochondrosis is important to avoid many problems.
diagnosis
To establish the diagnosis, the patient is referred to an instrumental examination:
- Roentgen;
- Duplex scanning;
- Ultrasound dopplerography;
- Computed or magnetic resonance imaging.
Diagnostic measures provide information about the location and extent of the damage.
First aid
In the event that the patient experiences excruciating pain, pain relievers (metamizole sodium, etc. ) will come to the rescue. If they can't get rid of the pain, they resort to non-steroidal anti-inflammatory drugs (diclofenac, ibuprofen, nimesulide). However, they cannot be taken for a long time because they have a negative effect on the intestines.
Anesthetic ointments with a warming effect and a pepper plaster can effectively relieve pain.
If the patient's limbs become numb, massage and special exercises to activate blood circulation are recommended.
With edema, diuretics are taken.
However, all of the above means can only have a temporary effect. Therefore, to prevent complications from developing, you should not postpone the visit to the doctor.
Treatment methods

In order for the fight against the disease to be crowned with success, it is necessary:
- relieve pain syndrome;
- Remove puffiness;
- restore blood flow;
- strengthen the muscle corset;
- improve tissue nutrition and ensure their regeneration.
Treatment for cervical osteochondrosis should be comprehensive and include:
- Drug therapy;
- Physical therapy;
- physiotherapy exercises;
- Methods of alternative and traditional medicine;
- Diet.
Drug treatment includes taking:
- anti-inflammatory drugs - relieve inflammation, relieve pain, activate blood circulation;
- Muscle relaxants - relieve muscle spasms;
- Chondroprotectors - restore the cartilage tissue;
- B vitamins - both oral and intramuscular administration are possible.
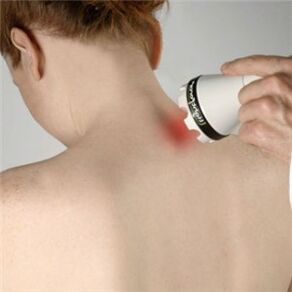
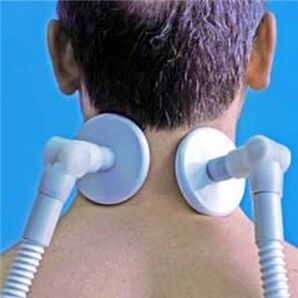
Physiotherapeutic procedures have an effective effect on cervical osteochondrosis:
- Magnetic therapy;
- Electrophoresis;
- Water therapy;
- Paraffin therapy.
Effective help in the fight against the disease is provided by non-traditional methods (osteopathy, homeopathy, reflexology, hirudotherapy), massage, manual therapy and special exercises. They stimulate blood circulation, relieve muscle tension, which has a positive effect on the general condition of the body. But it is necessary to do physical therapy exercises under the supervision of a specialist, otherwise you can get the opposite effect.
In addition to (but not instead of) drug treatment, it is recommended to use folk remedies.
For 3-4 months you need to follow a strict diet:
- Waste products containing cholesterol: animal fats, fatty meat;
- limit the consumption of sugar, salt, flour products;
- Exclude alcoholic beverages.
prophylaxis

An active lifestyle and weight loss are key preventative measures. A diet that contains the necessary vitamins and minerals is of no small importance.
The sleeping mattress should be firm and the pillow should be low.
Make sure you take breaks when you are seated.
People prone to osteochondrosis need to see an orthopedic surgeon regularly.















































